ALGORITHM
NOTE: Please also be sure the statement in this window matches statement you are addressing within the survey.
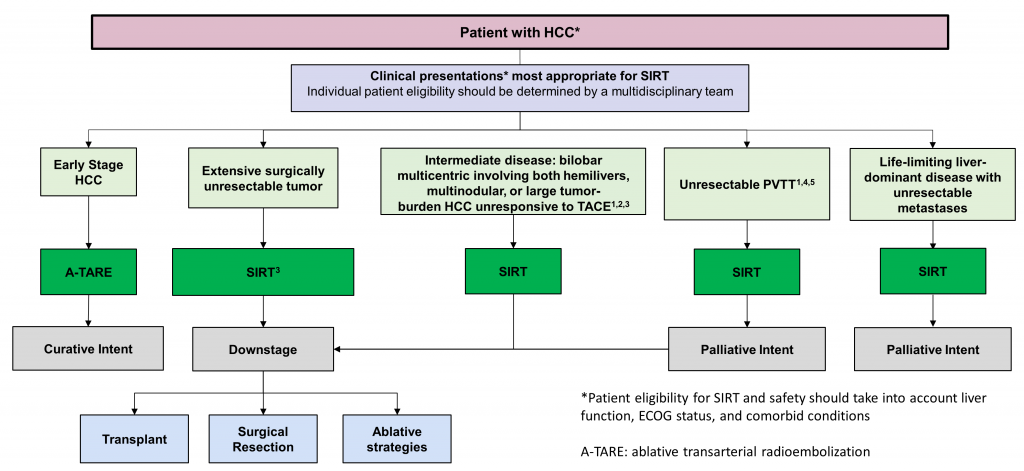
2. SIRT is recommended for the 5 categories of patients with HCC shown in the algorithm:
- Chen et al. Pan-Asian adapted ESMO Clinical Practice Guidelines for the management of patients with intermediate and advanced/relapsed hepatocellular carcinoma. Ann Oncol 2020 Mar;31(3):334-351, https://doi.org/10.1016/j.annonc.2019.12.001
- Park et al. Consensus for Radiotherapy in Hepatocellular Carcinoma from The 5th Asia-Pacific Primary Liver Cancer Expert Meeting (APPLE 2014): Current Practice and Future Clinical Trials. Liver Cancer 2016;5:162-174, https://doi.org/10.1159/000367766
- Lau et al. Patient selection and activity planning guide for selective internal radiotherapy with yttrium-90 resin microspheres. Int J Radiation Oncology Biol Phys (2012) 82:401-407, https://doi.org/10.1016/j.ijrobp.2010.08.015
- Cheng et al. Chinese Expert Consensus on Multidisciplinary Diagnosis and Treatment of Hepatocellular Carcinoma with Portal Vein Tumor Thrombus (2018 Edition). Liver Cancer 2020;9:28–40, https://doi.org/10.1159/000503685
- Taiwan groups. Management consensus guideline for hepatocellular carcinoma: 2016 updated by the Taiwan Liver Cancer Association and the Gastroenterological Society of Taiwan. J Formos Med Assoc 2018 May;117(5):381-403, https://doi.org/10.1016/j.jfma.2017.09.007
SIR-Spheres Y-90 resin microspheres. Prescribing information PI-EC-13. Sirtex Medical Inc; 2019. www.sirtex.com/media/169278/pi-ec-13-spheres-ifu-eu-row.pdf
3. Early-stage HCC is defined following Milan criteria for SIRT with curative intent: (1) single tumor diameter < 5 cm; (2) ≤ 3 foci of tumor, each one ≤ 3 cm; (3) no angioinvasion; (4) no extrahepatic involvement.
References: SIRT with resin microspheres in non-Asian regions
Article
Grade
Key Points
Gordon-Weeks et al. Systematic review of outcome of downstaging hepatocellular cancer before liver transplantation in patients outside the Milan criteria. Br J Surg. 2011 Sep;98(9):1201-8. doi: 10.1002/bjs.7561
C-LD
- Systematic literature review of studies (United States, Korea, Germany, Italy, Austria) (rated as low quality in the review) reporting the outcomes of HCC patients outside the Milan criteria who underwent downstaging before liver transplants
- 8 observational studies identified for analysis. These studies encompass 720 patients treated with a range of downstaging procedures
- Of these 720 patients, 6 underwent SIRT treatment in combination with other downstaging procedures (TACE and/or radiofrequency ablation and/or resection)
- Overall, the rate of successful downstaging varied from 24-69%
- Overall, survival rates ranged from 82-100% at 1-year post-transplant, 79-100% at 3-years post-transplant, and 54.6-94% at 5-years post-transplant
- Taken overall, survival rates of patients who did not initially meet Milan criteria but who underwent liver transplants after successful downstaging are comparable to the survival rates of patients within the Milan criteria
4. Intermediate-stage HCC is defined as not meeting Milan criteria for early-stage disease but without macrovascular invasion or extrahepatic spread; and multinodular disease as more than three foci of tumor, each one not exceeding 3 cm.
5. The following situations constitute locally advanced disease: tumor size >10 cm, previous curative ablation/surgery with recurrence, previous radiation exposure (e.g., EBRT/SBRT/SABER, SIRT), progression on systemic therapy.
6. In formulating statements about intermediate and locally advanced HCC, we would like your input into how to best differentiate these disease states: How do you differentiate between intermediate and locally advanced HCC in the setting of bilobar multicentric non-surgical disease?
7. Suitability for surgical resectability should be decided by the surgical team and/or institution.
8. Treatment of early-stage HCC with ablative transarterial radioembolization (A-TARE) has curative intent.
References: SIRT with resin microspheres in Asian regions
Article
Grade
Key Points
B-NR
- Meta-analysis of 2 RCTs and 9 observational studies conducted in Germany, Spain, China, Egypt, Turkey, USA: 1652 patients with unresectable HCC treated with SIRT (resin and/or glass)
- HBV: 14.1% in TACE, 12.9% in SIRT; HCV: 32.1% in TACE, 40.7% in SIRT
- Liver function was assessed and reported for each paper; no differences were found in patient characteristics among the trials
- 1-year and 2-year survival rates were analyzed based on observational or RCT study design; 1-year rates were similar, but 2-year rates were higher for SIRT than TACE treated patients
- Tumor responses were assessed using either WHO (n=4) or mRECIST (n=5), the significant differences varied depending on type of analysis used (mRECIST)
- Serious AEs (≥grade 3) were rare and did not differ between treatments
B-NR
- Retrospective multi-center (South Korea) case series of HCC patients (n=50), BCLC stages A—C (20% HCV, 66% HBV), treated with SIRT (resin)
- Study aim was to specifically evaluate safety, efficacy, and outcomes of SIRT treatment in a population of Asian patients (treated in South Korea), a majority of whom had chronic HBV infections
- 40% of patients showed a response to treatment while 46% achieved stable disease. BCLC stage was significantly associated with overall response rate (ORR) (p=0.003)
- Median overall survival (OS) for the entire cohort was 40.9 months (95% CI, 10.2–71.6 months). For patients with BCLC stage A, median survival was not reached, but the mean survival time was 39.4 months. For patients with BCLC stage B, median OS was 42.4 months (95% CI, 22.9–86 months), and for patients with BCLC stage C, median OS was 17.9 months (95% CI, 11.2–24.7 months)
- In univariate analysis, BCLC stage, Child-Pugh Score, PVT, and tumor response were significantly associated with survival
- Median time-to-progression (TTP) for the group overall was 5.9 months (range 0.9—46.1 months)
- Follow-up treatments were conducted in 31 patients due to remnant HCC or HCC progression; these follow-up treatments included TACE, RFA, surgery, radiation treatment, and combination treatments
- SIRT treatment appears to be well tolerated and effective in Asian patients with early to intermediate stage BCLC, and follow-up treatments post-SIRT were safely provided in this population
C-LD
- Retrospective single-center (Hong Kong) study of outcomes in patients with inoperable HCC who received SIRT treatment (n=30) (resin) compared to those who did not (n=16)
- HCV/HBV infection rates of patients were not specified
- MAA assessment was performed in both groups and survival time was calculated from that date
- Median overall survival (OS) was >31.9 months for patients with BCLC A stage disease, 14.5 months for patients with BCLC B, and 5.2 months for patients with BCLC C
- Among patients with BCLC C, SIRT treatment was associated with significantly longer median OS (5.2 months vs 3.8 months, p=0.047
- SIRT was also significantly associated with longer OS among patients with PVT (5.2 months vs 3.8 months, p=0.04) and patients who had less than 3 nodules (10.6 months vs 3.3 months, p=0.004)
- Multivariate analysis identified independent factors for survival as Child-Pugh class, tumor diameter sum, BCLC stage, and SIRT treatment
- Radioembolization-induced liver disease (REILD) was reported in 13% of patients
- SIRT may improve survival for certain subgroups of patients with inoperable HCC, but caution should be taken for the possible complication of REILD
C-LD
- Retrospective multi-center case series (Asia-Pacific, Europe, USA) of patients with HCC (or other malignancies) receiving SIRT with resin microspheres, followed by liver transplantation or resection
- Patient characteristics included bilobar (n=44), cirrhosis (n=41), total bilirubin grade ≥1 (n=28)
- Intent of SIRT was bridge (n=9) downstaging or palliative (n=84) or not available (n=7)
- Median IQR total SIRT activity was 1.5 GBq
- Median time to LT was 10.1 months and to surgery, 5.7 months
- Complete resection was achieved in 54 patients, R1 in 15, and R2 in 2
- 25 resected patients had exposure of the FLR to SIRT, 3 had partial exposure of the FLR to SIRT; 32 had whole liver SIRT
- 78 patients did not have post-SIRT chemotherapy
References: SIRT with resin microspheres in non-Asian regions
Article
Grade
Key Points
B-R
- Multi-center open-label pilot RCT conducted in Germany on patients with unresectable HCC receiving SIRT with resin microspheres
- Patients randomized to receive either SIRT (n=13) or TACE (n=15)
- Patient characteristics included ECOG 0/1 (SIRT, n=10/3; TACE, n=12/3); Child Pugh 5/6/7 (SIRT, n=9/3/1; TACE, n=9/4/2); AFP mean (SIRT, 636 ng/dL; TACE, 2624.7 ng/dL); total bilirubin median IQR (SIRT 1; TACE 1.08); Albumin median IQR (SIRT 3.63; TACE 4.20); BCLC A/B/C (SIRT, n=5/5/3; TACE, n=4/8/3)
- Median activity 1.6 GBq delivered to whole (n=7), lobe (n=5), or segment (n=1)
- No difference in QoL measures were detected 12 weeks after treatment
- Using RECIST 1.0, PR was 30.8% for SIRT and 13.3% for TACE; 2 patients in each group were downstaged for LT (n=3) or RFA (n=1)
- Median PFS was 3.6 months for SIRT and 3.7 months for TACE
- No differences in frequency of AE between groups; only GI events occur more frequently in SIRT group; SAE occurred in 7 and 5 patients, respectively
B-NR
- Retrospective single-center (Canada) study of patients with advanced HCC with PVTT treated with SIRT (resin or glass)
- Cohorts treated with ablative intent transarterial radioembolization (A-TARE, n=21), or conventional technique (cTARE, n=36)
- Dosimetry resin (partition model): >70 Gy to liver parenchyma with A-TARE, >100 Gy to tumor with cTARE
- Dosimetry glass (MIRD model): >190 Gy to total volume with A-TARE, >120 Gy to total volume with cTARE
- A-TARE was associated with longer median OS (45.3 vs 18.2 months; P = 0.003), longer post-treatment survival
- (19.1 vs 4.9 months; P = 0.005), a 70% lower risk of death (hazard ratio 0.30; 95% CI, 0.13–0.70; P = 0.005), and improved 4-year survival (53.9% vs 11.2%) than cTARE
- Overall survival did not differ between resin and glass microspheres (27.5 vs 22.2 months; P = 0.62)
B-NR
- Retrospective SEER analysis of 189 patients (USA) with unresectable HCC who were treated with SIRT using resin microspheres (n=77) or treated with SBRT (n=112)
- Etiology not specified
- Median overall survival (OS) for SIRT-treated patients was 12 months (95% CI: 9–17) vs 14 months (95% CI: 10–18) for patients treated with SBRT
- Disease-specific survival (DSS) for SIRT-treated patients was 14 months (95% CI: 10–22) vs 14 months (95% CI: 12–20) for patients treated with SBRT
- After adjustment for confounding factors, no significant differences were seen between treatment groups for OS (hazard ratio (HR), 0.72; 95% CI, 0.49–1.07; p=0.1077) or DSS (HR, 0.70; 95% CI, 0.46–1.05; p=0.0880)
- For both treatment groups, elevated AFP levels were significantly associated with higher risk of death (p=0.0459) and disease-specific risk of death (p=0.0233)
C-LD
- Retrospective single-center case series (Italy) of 22 patients with HCC undergoing liver transplant after SIRT with resin microspheres
- Patient characteristics included hepatitis B/C (n= 2/17); BCLC A/B/C (n=3/15/4); before SIRT within Milan criteria (n=3); at LT within Milan criteria (n=18)
- Using mRECIST, CR/PR/SD/PD was 9/9/1/2
- Median activity delivered was 1.6 GBq
- MELD score increased for 11 patients within 6 months after SIRT and remained stable for 11 patients
- AFP decreased in all cases after SIRT
- Downstaging occurred for 19 patients and 3 had successful bridge to LT
- OS from SIRT was 43.9 months and from LT was 30.2 months
C-LD
- Retrospective single-center case series (UK) of patients with unresectable HCC receiving SIRT with glass or resin microspheres, followed by liver resection
- All had normal bilirubin (5.0 to 17.0 mmol/L)
- Time from SIRT to resection: mean 322 days (range 195–703)
- Resected margins were R0 (n=4), R1 (n=5)
- Mean increase in FLR was 264 cm3
- Clavien-Dindo classification was II (n=5) III (n=7), IV (n=2), V (n=1)
C-LD
- Retrospective single-center case series (USA) of 111 patients (59.1% HCV, 8.2% HBV) treated with SIRT (resin) for unresectable HCC
- Median overall survival (OS) was 13.1 months (95% CI, 10.3–18.4), and median survival without progression in the liver (liver PFS) was 9.8 months (95% CI, 6.8–14.8)
- A number of factors were significantly associated with longer OS. These included absence of bilobar disease, absence of PVT, early stage BCLC disease vs later stage, absence of ascites, sorafenib treatment, and treatment with other liver-directed locoregional treatments in addition to SIRT
- In 6 patients, SIRT was used as a bridge to liver transplantation, which resulted in greatly improved survival compared to patients who did not undergo liver transplants (69.0 months vs 12.1 months, respectively; p=0.001)
- 21.5% of patients experienced treatment-related adverse events (AEs) 1 week after SIRT, and 43.4% experienced these 3 months after SIRT. The most common AEs reported were abdominal pain, ascites, nausea, and edema
9. Patients with post-non-radiation HCC recurrence without transplant capabilities should be amenable to SIRT, provided they have adequate hepatic function. In the case of patients with HCC recurrence following SIRT or other radiation therapies, appropriate calculations of exposure may be warranted with palliative intent.
References: SIRT with resin microspheres in non-Asian regions
Article
Grade
Key Points
B-NR
- Systematic review of 7 retrospective studies conducted in China, Hong Kong, Taiwan, Japan and France comparing salvage liver transplantation (n=158) and curative locoregional therapy (n=682) for treatment of recurrent HCC
- Repeat hepatectomy was used in 6 studies, RFA in 4, TACE in 2, PEI in 2. There is no mention of use of SIRT
- No significant difference was found in 1- and 3-year OS, but salvage liver transplantation had better 5-year OS
C-LD
- Single-center (China) retrospective analysis of 397 patients with HCC, 177 of them with recurrent HCC
- Etiology: 282 patients had HBV infection and 39 had HCV infection
- Patients with recurrence underwent re-resection (n=18), RFA (n=4), TACE (n=98), sorafenib (n=11) or conservative management (n=46)
- No patient received SIRT
References: SIRT with resin microspheres in non-Asian regions
Article
Grade
Key Points
C-LD
- Single-center (Switzerland) retrospective analysis of 147 patients with HCC, 67 of them with recurrent HCC (14 had cirrhosis of viral etiology)
- Patients with recurrent HCC and were treated with a variety of approaches: palliative care, RFA, TACE, repeat hepatectomy, etc
- Only 1 patient was treated with SIRT, but no details are provided
10. PVTT should be subcategorized for better assessment of patient prognosis and survival.
References: SIRT with resin microspheres in non-Asian regions
Article
Grade
Key Points
C-EO
- Clinical consensus statement from experts in China on HCC with PVTT
- Doctors in China tend to use more curable treatments for PVTT patients
- PVTT should be diagnosed with Cheng’s classification
- Different multidisciplinary treatments are recommended taking into account liver function (Child–Pugh), resectability, extrahepatic metastasis, and extent of PVTT
- Surgery is the preferred option for patients with type I/II PVTT. Type III can undergo resection after downstaging with TACE and/or radiotherapy
- SIRT is recommended for patients with unresectable primary tumors; PVTT types I–III; and Child–Pugh A liver function
11. Extensive surgically unresectable tumors should treated with SIRT aiming to downstage, which may be followed by transplant, surgical resection or ablative therapies.
References: SIRT with resin microspheres in Asian regions
Article
Grade
Key Points
B-NR
- Open-label Phase I and II study (Hong Kong) to determine optimum dose of radiation and response and complication rates from use of SIRT (resin) in the treatment of inoperable HCC
- 18 patients with inoperable HCC (etiology unknown) were treated with SIRT
- Median survival was significantly improved for patients whose tumors received >120 Gy compared to patients whose tumors received lower doses (55.9 weeks vs 26.2 weeks, respectively; p=0.005)
- Partial response was seen in 7/8 patients who received >120 Gy to all tumors compared to 1/8 patients who received <120 gy to at least one nodule. This difference in response rates was statistically significant (p=0.005)
- SIRT treatment was well tolerated without major complications, and a tumor dose of >120 Gy is recommended
B-NR
- Meta-analysis of 2 RCTs and 9 observational studies conducted in Germany, Spain, China, Egypt, Turkey, USA: 1652 patients with unresectable HCC treated with SIRT (resin and/or glass)
- HBV: 14.1% in TACE, 12.9% in SIRT; HCV: 32.1% in TACE, 40.7% in SIRT
- Liver function was assessed and reported for each paper; no differences were found in patient characteristics among the trials
- 1-year and 2-year survival rates were analyzed based on observational or RCT study design; 1-year rates were similar, but 2-year rates were higher for SIRT than TACE treated patients
- Tumor responses were assess using either WHO (n=4) or mRECIST (n=5), the significant differences varied depending on type of analysis used (mRECIST)
- Serious AEs (≥grade 3) were rare and did not differ between treatments
C-LD
- Retrospective multi-center case series (Asia-Pacific, Europe, USA) of patients with HCC (or other malignancies) receiving SIRT with resin microspheres, followed by liver transplantation or resection
- Patient characteristics included bilobar (n=44), cirrhosis (n=41), total bilirubin grade ≥1 (n=28)
- Intent of SIRT was bridge (n=9) downstaging or palliative (n=84) or not available (n=7)
- Median IQR total SIRT activity was 1.5 GBq
- Median time to LT was 10.1 months and to surgery, 5.7 months
- Complete resection was achieved in 54 patients, R1 in 15, and R2 in 2
- 25 resected patients had exposure of the FLR to SIRT, 3 had partial exposure of the FLR to SIRT; 32 had whole liver SIRT
- 78 patients did not have post-SIRT chemotherapy
C-LD
- Prospective multi-center case series (South Korea) of 40 patients with HCC (12.5% HCV, 80% HBV) treated with SIRT (resin)
- Median time to progression was 18 months and overall 3-year survival rate was 75%. For patients with BCLC B stage disease (n=19), the 3-year survival rate was 50%
- At 3 months, the overall response rate was 57.5% (23/40), and disease control rate was 95% (38/40). At 6 months, the response rate was 63.9% (23/36), and the disease control rate was 83.3% (30/36)
- Tumor number was significantly associated with patient survival after SIRT treatment
- Adverse events were manageable, with mild-to-moderate abdominal pain as the most frequent
C-LD
- Case series analysis of outcomes for 71 patients (Hong Kong) with unresectable HCC (91% HBV) who received SIRT treatment with resin microspheres
- Median overall survival (OS) from date of diagnosis was 9.4 months (range 1.8 to 46.4 months)
- 51-87% reduction in tumor volume was seen in 26.7% of patients 4-10 months after first SIRT treatment
- Overall objective response, as assessed by changes in alpha-fetoprotein (AFP) levels, was 89% [partial response (PR) 67%, complete response (CR) 22%] among the 46 patients with raised pretreatment AFP levels
- Serum ferritin levels were used to evaluate treatment response in the 25 patients without elevated pretreatment AFP levels. Ferritin levels dropped 34-99% after treatment, with a median of 62%
- 4 patients underwent surgical resection after SIRT treatment, with 2 showing complete histological remission
- SIRT treatment was well tolerated, with no symptoms of radiation hepatitis, pneumonitis, or bone-marrow toxicity
C-LD
- Retrospective single-center (Singapore) analysis of 103 patients with HCC (23.3% HCV, 47.6% HBV) treated with SIRT (resin)
- Patients were typically unsuitable for surgical resection, and typically of intermediate or advanced stage disease (BCLC B or BCLC C stage)
- Median overall survival (OS) for the entire cohort was 14.4 months (95 % CI 11.0–22.2)
- Patients with Child-Pugh (CP) class A disease had significantly better median OS compared to patients with Child-Pugh class B disease (21.7 months vs 7.1 months, respectively; p=0.0001)
- Hepatitis C, pretreatment vascular invasion, low serum albumin, and elevated levels of total bilirubin levels were all significantly associated with poorer overall survival
- Disease control of treated lesions was 100%; however, 37% of patients eventually developed progressive disease due to the development of new lesions, local extension of tumor into the vasculature, or both
C-LD
- Retrospective single-center (Hong Kong) study of outcomes in patients with inoperable HCC who received SIRT treatment (n=30) (resin) compared to those who did not (n=16)
- HCV/HBV infection rates of patients were not specified
- MAA assessment was performed in both groups and survival time was calculated from that date
- Median overall survival (OS) was >31.9 months for patients with BCLC A stage disease, 14.5 months for patients with BCLC B, and 5.2 months for patients with BCLC C
- Among patients with BCLC C, SIRT treatment was associated with significantly longer median OS (5.2 months vs 3.8 months, p=0.047.
- SIRT was also significantly associated with longer OS among patients with PVT (5.2 months vs 3.8 months, p=0.04) and patients who had less than 3 nodules (10.6 months vs 3.3 months, p=0.004)
- Multivariate analysis identified independent factors for survival as Child-Pugh class, tumor diameter sum, BCLC stage, and SIRT treatment
- Radioembolization-induced liver disease (REILD) was reported in 13% of patients
- SIRT may improve survival for certain subgroups of patients with inoperable HCC, but caution should be taken for the possible complication of REILD
C-EO
- Clinical practice guideline by experts from Japan, Taiwan, South Korea, China, India, Pakistan, Indonesia, Philippines on HCC
- SIRT is considered for:
- Unresectable HCC: as an alternative locoregional therapy
- Patients who are not suitable candidates for TACE due to bulky tumor and/or portal vein invasion
References: SIRT with resin microspheres in non-Asian regions
Article
Grade
Key Points
B-R
- Multi-center open-label pilot RCT conducted in Germany on patients with unresectable HCC receiving SIRT with resin microspheres
- Patients randomized to receive either SIRT (n=13) or TACE (n=15)
- Patient characteristics included ECOG 0/1 (SIRT, n=10/3; TACE, n=12/3); Child Pugh 5/6/7 (SIRT, n=9/3/1; TACE, n=9/4/2); AFP mean (SIRT, 636 ng/dL; TACE, 2624.7 ng/dL); total bilirubin median IQR (SIRT 1; TACE 1.08); Albumin median IQR (SIRT 3.63; TACE 4.20); BCLC A/B/C (SIRT, n=5/5/3; TACE, n=4/8/3)
- Median activity 1.6 GBq delivered to whole (n=7), lobe (n=5), or segment (n=1)
- No difference in QoL measures were detected 12 weeks after treatment
- Using RECIST 1.0, PR was 30.8% for SIRT and 13.3% for TACE; 2 patients in each group were downstaged for LT (n=3) or RFA (n=1)
- Median PFS was 3.6 months for SIRT and 3.7 months for TACE
- No differences in frequency of AE between groups; only GI events occur more frequently in SIRT group; SAE occurred in 7 and 5 patients, respectively
B-NR
- Retrospective SEER analysis of 189 patients (USA) with unresectable HCC who were treated with SIRT using resin microspheres (n=77) or treated with SBRT (n=112)
- Etiology not specified
- Median overall survival (OS) for SIRT-treated patients was 12 months (95% CI: 9–17) vs 14 months (95% CI: 10–18) for patients treated with SBRT
- Disease-specific survival (DSS) for SIRT-treated patients was 14 months (95%
CI: 10–22) vs 14 months (95% CI: 12–20) for patients treated with SBRT - After adjustment for confounding factors, no significant differences were seen between treatment groups for OS (hazard ratio (HR), 0.72; 95% CI, 0.49–1.07; p=0.1077) or DSS (HR, 0.70; 95% CI, 0.46–1.05; p=0.0880)
- For both treatment groups, elevated AFP levels were significantly associated with higher risk of death (p=0.0459) and disease-specific risk of death (p=0.0233)
B-NR
- Retrospective single-center cohort study (Spain) of 21 patients with HCC stage UNOS T3 who received SIRT treatment (resin).
- Survival outcomes were compared between patients who were successfully downstaged to receive radical treatments (resection, transplantation, or radiofrequency ablation plus resection) after SIRT and patients who did not receive radical therapy after SIRT
- 6 patients were successfully downstaged and treated radically 2–35 months post-SIRT. These patients were significantly younger than the rest (62 years vs 73 years, p=0.006) and also had significantly higher tumor volumes (583 mL vs. 137 mL, p = 0.001)
- Median overall survival (OS) for all patients was 27 months (95% CI 5.0-48.9), and varied significantly between patients who received radical treatment (not reached after a median follow-up of 48.0 months post-SIRT and 41.5 months post-radical therapy) and the patients who did not receive radical treatment (22 months; 95% CI 15.0-30.9)
- For a select subgroup of UNOS T3 stage HCC patients, SIRT treatment followed by radical therapy offers the possibility of long-term survival
B-NR
- Retrospective cohort study (prospectively collected data) (Switzerland) of patients with unresectable HCC treated with SIRT (resin or glass)
- HBV: 12.2% in resin group, 8.3% in glass group. HCV: 29.3% in resin group, 19.4% in glass group
- Median administered activity was calculated using the partition model for resin (1.8 GBq) and using 2-compartment model for glass (1.8 GBq)
- In the resin group, 90Y tumor-absorbed dose was 160 Gy, normal liver-absorbed dose was 36 Gy
- PFS and OS for resin were higher than for glass but not statistically significant
- No survival differences were detected when BCLC stages early/intermediate and advanced were compared
- BCLC staging and serum AFP were associated with PFS for glass only
B-NR
- Retrospective single-center cohort study (USA) of patients with unresectable HCC treated with SIRT (resin) or TACE
- Patient characteristics included hepatitis C (SIRT, n=10; TACE, n=25); Child Pugh A/B (SIRT, n=13/14; TACE n=22/22); MELD score (SIRT, 10.0; TACE, 10.4); Okuda I/II/III (SIRT, n=13/13/1; TACE, n=15/27/3); vascular invasion (SIRT, n=14; TACE n=13); mean AFP level ug/L (SIRT, 801; TACE, 690)
- Activity calculated by BSA method
- Using RECIST and evaluated after 4 and then every 12 weeks, CR/PR/SD/PD were 0/3/11/9 for SIRT and 1/2/16/16 for TACE
- Median survival was 6.0 months for both SIRT and TACE
- No differences were found for any complications or major complications between groups. Hematologic specific complications different between treatments: SIRT had 0 and TACE had 10
C-LD
- Case series analysis of 30 patients (India) treated with SIRT (resin) for primary unresectable HCC (etiology not specified, n=21) or hepatic metastases from other solid tumors (colorectal cancer: 7, melanoma: 1; ovarian carcinoma: 1)
- At 3 months follow-up, a complete response wa observed in 7% of patients (2/30), partial response in 23% (7/30), stable disease in 50% (15/30), and progressive disease in 20% (6/30)
- 46% (14/30) of patients developed minor side effects from SIRT therapy, all of which were resolved with conservative management. The most common adverse events were mild abdominal pain, nausea, and fatigue
- There is supportive evidence for the safety and efficacy of SIRT in the treatment of primary unresectable HCC and hepatic metastases from other primary cancers
C-LD
- Retrospective single-center (Turkey) analysis of 78 patients treated with SIRT (resin) for unresectable liver tumors from primary HCC (etiology not specified, n=25) or unresectable hepatic metastases from other primary tumors (colorectal: 35; gastric: 7; breast: 4; malign melanoma: 1; pancreas: 1; renal cell: 1; esophagus: 1; neuroendocrine: 3)
- Patients were classified into two groups according to their disease stage: those with only liver metastases (H) and those in which metastases had spread to other organs (EH)
- As assessed by FDG-PET/CT in the sixth week after SIRT treatment, 55% of patients showed a metabolic treatment response while 45% of patients were classified as non-responders
- 31% of non-responding patients had H disease (tumors restricted to the liver i.e. no extrahepatic metastases) but 69% of responders had H disease (p < 0.05)
- The mean overall survival of those in the “responders” group was significantly longer than those in the non-responding group: 25.63 ± 1.52 months vs 20.45 ± 2.11 months, respectively (p = 0.04)
- SIRT may be a useful treatment for patients with both primary and metastatic unresectable liver tumors, and FDG-PET/CT may be a successful imaging method for evaluating treatment response and predicting survival time
C-LD
- Retrospective single-center case series (Italy) of 22 patients with HCC undergoing liver transplant after SIRT with resin microspheres
- Patient characteristics included hepatitis B/C (n= 2/17); BCLC A/B/C (n=3/15/4); before SIRT within Milan criteria (n=3); at LT within Milan criteria (n=18)
- Using mRECIST, CR/PR/SD/PD was 9/9/1/2
- Median activity delivered was 1.6 GBq
- MELD score increased for 11 patients within 6 months after SIRT and remained stable for 11 patients
- AFP decreased in all cases after SIRT
- Downstaging occurred for 19 patients and 3 had successful bridge to LT
- OS from SIRT was 43.9 months and from LT was 30.2 months
C-LD
- Prospective single-center case series (Italy) of 24 patients with unresectable HCC and PVT were treated with SIRT (resin)
- 21% of these patients were successfully downstaged to surgery after SIRT treatment. 33% showed partial response or stable disease but were not eligible for surgery. The rest showed progressive disease.
- Median overall survival of patients was 70 months for the downstaged group, 24 months for those with partial response/stable disease, and 11 months for those with progressive disease.
- No serious adverse events (grades 3-4) were reported from SIRT treatment
C-LD
- Retrospective single-center case series (UK) of patients with unresectable HCC receiving SIRT with glass or resin microspheres, followed by liver resection
- All had normal bilirubin (5.0 to 17.0 mmol/L)
- Time from SIRT to resection: mean 322 days (range 195–703)
- Resected margins were R0 (n=4), R1 (n=5)
- Mean increase in FLR was 264 cm3
- Clavien-Dindo classification was II (n=5) III (n=7), IV (n=2), V (n=1)
C-LD
- Retrospective single-center case series (USA) of 111 patients (59.1% HCV, 8.2% HBV) treated with SIRT (resin) for unresectable HCC
- Median overall survival (OS) was 13.1 months (95% CI, 10.3–18.4), and median survival without progression in the liver (liver PFS) was 9.8 months (95% CI, 6.8–14.8)
- A number of factors were significantly associated with longer OS. These included absence of bilobar disease, absence of PVT, early stage BCLC disease vs later stage, absence of ascites, sorafenib treatment, and treatment with other liver-directed locoregional treatments in addition to SIRT
- In 6 patients, SIRT was used as a bridge to liver transplantation, which resulted in greatly improved survival compared to patients who did not undergo liver transplants (69.0 months vs 12.1 months, respectively; p=0.001)
- 21.5% of patients experienced treatment-related adverse events (AEs) 1 week after SIRT, and 43.4% experienced these 3 months after SIRT. The most common AEs reported were abdominal pain, ascites, nausea, and edema
Ince et al. Yttrium-90 (Y-90) Resin Microsphere Therapy for Patients with Unresectable Hepatocellular Carcinoma: a Single-Center Experience. J Gastrointest Cancer. 2017 Sep;48(3):281. doi: 10.1007/s12029-017-9968-z
C-LD
- Single-center (Turkey) case series of 28 patients with unresectable HCC treated with SIRT (resin). Meeting abstract
- As assessed by MRI or FDG PET/CT scans 2.5 months post-treatment, a complete response was seen in 7% of patients, a partial response in 36%, stable disease in 18%, and progressive disease in 39%
- Mean administered doses of Y90 to tumors, normal liver parenchyma and lungs were 105.7 ± 55.3, 25.5 ± 8.2, and 5.8 ± 1.7 Gy, respectively
- SIRT treatment was well-tolerated by patients, with no significant complications during the first week. One patient developed a treatment-related gastroduodenal ulcer 3 weeks post-treatment
- SIRT appears to be a safe and effective treatment option for unresectable HCC
12. Intermediate disease, characterized by bilobar multicentric disease involving both hemilivers, multinodular, or large tumor-burden HCC unresponsive to TACE should be treated with SIRT to downstage and can be followed by transplant, surgical resection or ablative therapies.
References: SIRT with resin microspheres in Asian regions
Article
Grade
Key Points
B-R
- Multi-center open-label RTC of SIRT (resin) vs sorafenib for Asian patients with locally advanced HCC
- Liver function parameters for inclusion: total bilirubin < 2.0mg/dL; INR ≤ 2.0; ALP ≤ 5 x institutional ULN; AST and ALT ≤ 5 x institutional ULN; albumin ≥ 2.5g/dL
- No difference in OS between SIRT and sorafenib, but better safety profile for SIRT than sorafenib
- Patient characteristics included ECOG 0/1 (SIRT, n=135/47; sorafenib, n=141/37) BCLC A/B/C (SIRT, n=0/93/88; sorafenib, n=1/97/80); Child Pugh A/B (SIRT, n=165/14; sorafenib, n=160/16); hepatitis B/C/B+C (SIRT, n=93/26/4; sorafenib, n=104/19/5)
- Activity administered was calculated by BSA or partition model and mean activity was 1.8 GBq
- Response was evaluated with RECIST 1.1
- Median daily dose was 644.5 mg sorafenib for patients who were planned to receive 400 mg twice daily
- ITT Median OS was 8.8 months for SIRT and 10.0 months for sorafenib; PP median OS was 11.3 month and 10.4 months; median PFS at any site was 5.8 and 5.1 respectively
- BCLC C treated population had median OS of 9.2 months for SIRT and 5.8 months for sorafenib (P=0.0475)
- Reported AEs were 437 events for SIRT and 1031 events for sorafenib
- Fewer SIRT patients than sorafenib patients experienced one or more AEs: 78 (60.0%) of 130 patients and 137 (84.6%) of 162 patients; AEs of grade ≥ 3: 36 (27.7%) and 82 (50.6%); or serious AEs (SAEs): 27 (20.8%) and 57 (35.2%)
C-LD
- Retrospective multi-center (South Korea) case series of HCC patients (n=50), BCLC stages A—C (20% HCV, 66% HBV), treated with SIRT (resin)
- Study aim was to specifically evaluate safety, efficacy, and outcomes of SIRT treatment in a population of Asian patients (treated in South Korea), a majority of whom had chronic HBV infections
- 40% of patients showed a response to treatment while 46% achieved stable disease. BCLC stage was significantly associated with overall response rate (ORR) (p=0.003)
- Median overall survival (OS) for the entire cohort was 40.9 months (95% CI, 10.2–71.6 months). For patients with BCLC stage A, median survival was not reached, but the mean survival time was 39.4 months. For patients with BCLC stage B, median OS was 42.4 months (95% CI, 22.9–86 months), and for patients with BCLC stage C, median OS was 17.9 months (95% CI, 11.2–24.7 months)
- In univariate analysis, BCLC stage, Child-Pugh Score, PVT, and tumor response were significantly associated with survival
- Median time-to-progression (TTP) for the group overall was 5.9 months (range 0.9—46.1 months)
- Follow-up treatments were conducted in 31 patients due to remnant HCC or HCC progression; these follow-up treatments included TACE, RFA, surgery, radiation treatment, and combination treatments
- SIRT treatment appears to be well tolerated and effective in Asian patients with early to intermediate stage BCLC, and follow-up treatments post-SIRT were safely provided in this population
C-LD
- Liver function was assessed and reported for each paper; no differences were found in patient characteristics among the trials
- 1-year and 2-year survival rates were analyzed based on observational or RCT study design; 1-year rates were similar, but 2-year rates were higher for SIRT than TACE treated patients
- Tumor responses were assess using either WHO (n=4) or mRECIST (n=5), the significant differences varied depending on type of analysis used (mRECIST)
- Serious AEs (≥grade 3) were rare and did not differ between treatments
C-LD
- Retrospective single-center cohort study (Hong Kong) of patients with unresectable advanced HCC treated with SIRT (resin) or TACE
- Patient characteristics included BCLC A/B (SIRT, n=15/1; TACE, n=14/2); hepatitis B/C (SIRT, n=12/0; TACE, n=13/3), AFP ng/mL (SIRT, 38; TACE, 242.5); albumin g/L (SIRT, n=40; TACE n=36.5); MELD (SIRT, 7.5; TACE 8.5); no portal invasion (SIRT, n=8; TACE, n=8)
- Using mRECIST and evaluating in 2 months, CR/PR/SD/PD were 0/4/5/7 for SIRT and 0/2/5/9 for TACE
- Median OS was 19.9 months for SIRT and 14.0 months for TACE (P=0.615)
- Despite title, not all patients had HBV (75% SIRT and 81.3% TACE)
C-LD
- Retrospective single-center (Korea) cohort study of patients with unresectable advanced HCC treated with either SIRT (resin) or SIRT with concurrent chemoradiation therapy (CCRT)
- Patient characteristics for the propensity score matching cohort included cirrhosis (SIRT, n=37; CCRT, n=35), Child Pugh B (SIRT, n=7; CCRT, n=2); BCLC B/C (SIRT, n= 12/50; CCRT, n=14/48); hepatitis B/C (SIRT, n=52/6; CCRT, n=50/2); AFP ng/mL (SIRT, n=216; CCRT, n=1291); PVT (SIRT, n=24; CCRT, n=33
- Using mRECIST, tumor response was determined at 1, 3, 6 months and 1 year after treatment
- Response was better in the CCRT than SIRT arm at 1 month (P<0.001) but was better in the SIRT arm than the CCRT at 3 months (P=0.04)
- By 6 months no differences were detected in tumor responses
- Median OS was 14.0 for SIRT and 13.2 for CCRT (P=0.435)
- Biochemical AEs were different between treatment groups. Overall, AEs occurred more frequently in the CCRT group than in the SIRT group
C-LD
- Systematic review and meta-analysis of RCTs on intermediate and locally-advanced HCC treated with SIRT or sorafenib and conducted in France, Spain, Italy, South Korea, and Singapore
- No significant differences in OS were found between SIRT and sorafenib, although subgroup analysis of patients with PVT showed superiority of SIRT in OS
- Disease control rate was similar with SIRT and sorafenib
- SIRT resulted in significantly higher ORR (29.3%) than sorafenib (8.4%), which has been considered a bridge option before liver transplantation or surgical resection
- Sorafenib led to a higher incidence of grade ≥3 events: fatigue, weight loss, diarrhea, and hypertension
- SIRT resulted in 1.7% radiation hepatitis
C-LD
- Systematic literature review of studies (United States, Korea, Germany, Italy, Austria) (rated as low quality in the review) reporting the outcomes of HCC patients outside the Milan criteria who underwent downstaging before liver transplants
- 8 observational studies identified for analysis. These studies encompass 720 patients treated with a range of downstaging procedures.
- Of these 720 patients, 6 underwent SIRT treatment (resin) in combination with other
- downstaging procedures (TACE and/or radiofrequency ablation and/or resection)
- Overall, the rate of successful downstaging varied from 24-69%
- Overall, survival rates ranged from 82-100% at 1-year post-transplant, 79-100% at 3-years post-transplant, and 54.6-94% at 5-years post-transplant
- Taken overall, survival rates of patients who did not initially meet Milan criteria but who underwent liver transplants after successful downstaging are comparable to the survival rates of patients within the Milan criteria
C-LD
- Retrospective multi-center case series (Asia-Pacific, Europe, USA) of patients with HCC (or other malignancies) receiving SIRT with resin microspheres, followed by liver transplantation or resection
- Patient characteristics included bilobar (n=44), cirrhosis (n=41), total bilirubin grade ≥1 (n=28)
- Intent of SIRT was bridge (n=9) downstaging or palliative (n=84) or not available (n=7)
- Median IQR total SIRT activity was 1.5 GBq
- Median time to LT was 10.1 months and to surgery, 5.7 months
- Complete resection was achieved in 54 patients, R1 in 15, and R2 in 2
- 25 resected patients had exposure of the FLR to SIRT, 3 had partial exposure of the FLR to SIRT; 32 had whole liver SIRT
- 78 patients did not have post-SIRT chemotherapy
C-LD
- Case series analysis of 30 patients (Hong Kong) treated with SIRT (resin) for advanced inoperable HCC (6.7% HCV, 70% HBV)
- Majorities of patients had chronic HBV infection and had been on antiviral therapy >4 years
- Median overall survival (OS) was 13.2 months and median progression-free survival (PFS) was 3.3 months
- Significantly longer median OS was seen in patients without PVT compared to those with PVT (17.1 months vs 4.4 months, p=0.015); for those whose duration of
- alfa-feto protein (AFP) response was >6 months vs those whose AFP response was shorter (21.2 months vs 8.6 months, p=0.001); and for treatment responders vs non-responders (21.2 months vs 8.6 months; P=0.015)
- Univariate analysis identified presence of PVT, response to treatment, and duration of AFP response >6 months as prognostic factors for OS
- Univariate analysis identified prior TACE treatment, tumor volume, response to treatment, and duration of AFP response>6 months as prognostic for progression-free survival (PFS)
- Treatment-related complications developed in 56.7% of patients, with grade 3 adverse events occurring in 16.7%. No higher-grade complications were reported
C-LD
- Retrospective single-center (Singapore) analysis of 103 patients with HCC (23.3% HCV, 47.6% HBV) treated with SIRT (resin)
- Patients were typically unsuitable for surgical resection, and typically of intermediate or advanced stage disease (BCLC B or BCLC C stage)
- Median overall survival (OS) for the entire cohort was 14.4 months (95 % CI 11.0–22.2)
- Patients with Child-Pugh (CP) class A disease had significantly better median OS compared to patients with Child-Pugh class B disease (21.7 months vs 7.1 months, respectively; p=0.0001)
- Hepatitis C, pretreatment vascular invasion, low serum albumin, and elevated levels of total bilirubin levels were all significantly associated with poorer overall survival
- Disease control of treated lesions was 100%; however, 37% of patients eventually developed progressive disease due to the development of new lesions, local extension of tumor into the vasculature, or bot
C-LD
- Prospective multi-center case series (South Korea) of 40 patients with HCC (12.5% HCV, 80% HBV) treated with SIRT (resin)
- Median time to progression was 18 months and overall 3-year survival rate was 75%. For patients with BCLC B stage disease (n=19), the 3-year survival rate was 50%
- At 3 months, the overall response rate was 57.5% (23/40), and disease control rate was 95% (38/40). At 6 months, the response rate was 63.9% (23/36), and the disease control rate was 83.3% (30/36)
- Tumor number was significantly associated with patient survival after SIRT treatment
- Adverse events were manageable, with mild-to-moderate abdominal pain as the most frequent
C-LD
- Case series analysis of outcomes for 71 patients (Hong Kong) with unresectable HCC (91% HBV) who received SIRT treatment with resin microspheres
- Median overall survival (OS) from date of diagnosis was 9.4 months (range 1.8 to 46.4 months)
- 51-87% reduction in tumor volume was seen in 26.7% of patients 4-10 months after first SIRT treatment
- Overall objective response, as assessed by changes in alpha-fetoprotein (AFP) levels, was 89% [partial response (PR) 67%, complete response (CR) 22%] among the 46 patients with raised pretreatment AFP levels
- Serum ferritin levels were used to evaluate treatment response in the 25 patients without elevated pretreatment AFP levels. Ferritin levels dropped 34-99% after treatment, with a median of 62%
- 4 patients underwent surgical resection after SIRT treatment, with 2 showing complete histological remission
- SIRT treatment was well tolerated, with no symptoms of radiation hepatitis, pneumonitis, or bone-marrow toxicity
C-LD
- Retrospective single-center (Hong Kong) study of outcomes in patients with inoperable HCC who received SIRT treatment (n=30) (resin) compared to those who did not (n=16)
- HCV/HBV infection rates of patients were not specified
- MAA assessment was performed in both groups and survival time was calculated from that date
- Median overall survival (OS) was >31.9 months for patients with BCLC A stage disease, 14.5 months for patients with BCLC B, and 5.2 months for patients with BCLC C
- Among patients with BCLC C, SIRT treatment was associated with significantly longer median OS (5.2 months vs 3.8 months, p=0.047.
- SIRT was also significantly associated with longer OS among patients with PVT (5.2 months vs 3.8 months, p=0.04) and patients who had less than 3 nodules (10.6 months vs 3.3 months, p=0.004)
- Multivariate analysis identified independent factors for survival as Child-Pugh class, tumor diameter sum, BCLC stage, and SIRT treatment
- Radioembolization-induced liver disease (REILD) was reported in 13% of patients
- SIRT may improve survival for certain subgroups of patients with inoperable HCC, but caution should be taken for the possible complication of REILD
C-EO
- Clinical consensus statement by experts from Taiwan on HCC
- BCLC should be used for prognostic prediction but other systems may be used in subgroups
- Prevention: vaccination for HBV, antiviral therapy (HBV, HCV), nucleotide/nucleoside analogues and interferon-based therapies
- SIRT is considered for:
- BCLC C stage patients with PVT
- Patients with major portal vein invasion, large tumor burden, or refractory to TAC
C-EO
- Clinical consensus statement on unresectable HCC by experts from China, Hong Kong, South Korea, Singapore, Taiwan
SIRT is considered in the following cases:
- Early-stage HCC (BCLC A): for bridging treatment for liver transplantation
- Intermediate-stage HCC (BCLC B: for bilobar, multinodular or large tumor burden, and also to treat patients after conventional TACE has failed. SIRT is also mentioned as a possible neoadjuvant treatment but there is limited data
- Advanced-stage HCC (BCLC C): for patients with vascular invasion and liver-dominant metastatic HCC
SIRT is also acknowledged as:
- Leading to favorable results regarding downsizing and objective response compared to TACE in some studies (intermediate HCC)
- Not associated with a strong embolic effect and, therefore, not contraindicated for patients with tumor thrombosis of major portal veins (advanced HCC)
Adverse events less likely with SIRT than TACE, but there are SIRT-specific complications
- SIRT contraindicated in tumor/normal liver ratios and high hepatopulmonary shunts
C-EO
- Clinical consensus statement by experts from Taiwan on HCC
- BCLC should be used for prognostic prediction but other systems may be used in subgroups
- Prevention: vaccination for HBV, antiviral therapy (HBV, HCV), nucleotide/nucleoside analogues and interferon-based therapies
- SIRT is considered for:
- BCLC C stage patients with PVT
- Patients with major portal vein invasion, large tumor burden, or refractory to TACE
C-EO
- Clinical practice guideline on intermediate and advanced/relapsed HCC by experts from Asia and Europe
- SIRT can be considered for:
- Intermediate- or advanced-stage HCC without extrahepatic disease: as first-line therapy alternative to TACE
- As an alternative for selected TACE-failed BCLC B or non-metastatic BCLC C patients. SIRT results in similar survival outcomes and better ORR and QoL compared to sorafenib in these patients
- For non-metastatic HCC with macrovascular invasion, which has shown benefit in some Asian studies, as well as other locoregional therapies (TACE, resection, HAIC)
- Advanced, non-metastatic patients: as locoregional therapy
- There is limited evidence on the improved benefit of using mRECIST over RECIST for predicting overall survival
C-EO
- Clinical practice guideline on HCC by experts from Singapore
- SIRT may be used in locally advanced HCC with no vascular invasion (level of evidence, 2b), as well as TACE, EBRT, and sorafenib
- Locoregional treatment such as TACE or SIRT can be considered for metastatic HCC with heavy liver tumor burden and good liver reserve
References: SIRT with resin microspheres in non-Asian regions
Article
Grade
Key Points
B-R
- Multi-center open-label RCT conducted in France on SIRT (with resin microspheres) vs sorafenib on locally advanced and unresectable HCC after unsuccessful TACE
- No significant difference in OS between SIRT and sorafenib
- Compared sorafenib 400 mg twice daily with SIRT to lobe, sector or segment
- Activity was calculated using BSA method
- Patient characteristics included hepatitis C/B (SIRT, n=55/13; sorafenib, n=49/15); ECOG 0/1 (SIRT, n=145/92; sorafenib, n=139/83); BCLC A/B/C (SIRT, n=9/66/162; sorafenib n=12/61/149); Child Pugh A(5-6)/B7/unknown (SIRT, n=196/39/2; sorafenib, n=187/35/0); bilobar (SIRT, n=50; sorafenib, n=35); macrovascular invasion (SIRT, n=149; sorafenib, n=128); AFP (SIRT, median 87 ng/mL, sorafenib, median 80.0 ng/mL)
- Activity delivered per patient was 1.394 GBq
- Median follow-up was 27.9 months in the SIRT group, 28.1 months in sorafenib group
- Response was evaluated with RECIST 1.1
- Median OS and PFS was 8.0 and 4.1 months for SIRT and 9.9 and 3.7 months for sorafenib
- Best overall response include CR (SIRT, n=5; sorafenib, n=2), PR (SIRT, n=31; sorafenib, n=21), SD (SIRT, n=93; sorafenib, n=131), PD (SIRT, n=60; sorafenib, n=44)
- 1088 serious adverse events were reported (SIRT, n=518 events; sorafenib, n=570 events)
B-R
- Multi-center open-label pilot RCT conducted in Germany on patients with unresectable HCC receiving SIRT with resin microspheres
- Patients randomized to receive either SIRT (n=13) or TACE (n=15)
- Patient characteristics included ECOG 0/1 (SIRT, n=10/3; TACE, n=12/3); Child Pugh 5/6/7 (SIRT, n=9/3/1; TACE, n=9/4/2); AFP mean (SIRT, 636 ng/dL; TACE, 2624.7 ng/dL); total bilirubin median IQR (SIRT 1; TACE 1.08); Albumin median IQR (SIRT 3.63; TACE 4.20); BCLC A/B/C (SIRT, n=5/5/3; TACE, n=4/8/3)
- Median activity 1.6 GBq delivered to whole (n=7), lobe (n=5), or segment (n=1)
- No difference in QoL measures were detected 12 weeks after treatment
- Using RECIST 1.0, PR was 30.8% for SIRT and 13.3% for TACE; 2 patients in each group were downstaged for LT (n=3) or RFA (n=1)
- Median PFS was 3.6 months for SIRT and 3.7 months for TACE
- No differences in frequency of AE between groups; only GI events occur more frequently in SIRT group; SAE occurred in 7 and 5 patients, respectively
B-NR
- Retrospective SEER analysis of 189 patients (USA) with unresectable HCC who were treated with SIRT using resin microspheres (n=77) or treated with SBRT (n=112)
- Etiology not specified
- Median overall survival (OS) for SIRT-treated patients was 12 months (95% CI: 9–17) vs 14 months (95% CI: 10–18) for patients treated with SBRT
- Disease-specific survival (DSS) for SIRT-treated patients was 14 months (95%
CI: 10–22) vs 14 months (95% CI: 12–20) for patients treated with SBRT - After adjustment for confounding factors, no significant differences were seen between treatment groups for OS (hazard ratio (HR), 0.72; 95% CI, 0.49–1.07; p=0.1077) or DSS (HR, 0.70; 95% CI, 0.46–1.05; p=0.0880)
- For both treatment groups, elevated AFP levels were significantly associated with higher risk of death (p=0.0459) and disease-specific risk of death (p=0.0233)
B-NR
- Retrospective single-center cohort study (Italy) of unresectable HCC to evaluate the efficacy and safety of SIRT treatment (resin) with relation to tumor morphology and extent of portal vein thrombosis (PVT)
- Retrospective analysis of 104 patients (80.8% HBV/HCV) with unresectable HCC treated with SIRT. ~60% had advanced BCLC stage C HCC, 50.0% had PVT, and 29.8% had infiltrative tumor morphology
- There was no significant difference in median overall survival (OS) between patients with segmental and patent portal vein PVT (17 months for both). However, OS did differ significantly between patients with patients with segmental PVT and lobar or main PVT (p = 0.031)
- Survival was more dependent on disease stage and liver function than size, number, distribution or morphology of the tumors
- There was no significant difference in median OS between patients with a nodular pattern of HCC and patients with an infiltrative pattern
- Prior TACE treatment and a treatment response at 3 months were both significantly correlated with improved OS
B-NR
- Retrospective single-center (Turkey) analysis of 80 patients who underwent SIRT (n=40) (resin) or TACE (n=40) for treatment of HCC (stage BCLC B or C)
- Although treatment groups were similar in most baseline characteristics, there was a significantly higher rate of chronic liver disease in the TACE treatment group (85%) than in the SIRT treatment group (55%), p=0.003. Rates of HCV/HBV infection were not given
- Mean OS Of the SIRT-treated group was significantly longer than mean OS of the TACE-treated group: 39.24±4.62 months (95% CI, 30.18–48.29 months) vs 30.63±3.68 months (95% CI, 23.42–37.84 months); p=0.014 and 2-year survival rates were 72% and 74% for the SIRT-treatment group and 47% and 59% for the TACE treatment group
- There was no significant difference between rates of disease recurrence or chronic complications between the two treatment groups
- For the SIRT treatment group, dimension of the largest lesion was a significant predictor of survival, while for the TACE treatment group, BCLC stage and female sex were significant predictors of survival
- Although there was a significantly longer mean OS for the SIRT treatment group vs the TACE treatment group, the significantly higher rate of chronic liver disease in the TACE treatment group should be considered as a factor that may influence survival
B-NR
- Retrospective single-center cohort study (USA) of patients with unresectable HCC treated with SIRT (resin) or TACE
- Patient characteristics included hepatitis C (SIRT, n=10; TACE, n=25); Child Pugh A/B (SIRT, n=13/14; TACE n=22/22); MELD score (SIRT, 10.0; TACE, 10.4); Okuda I/II/III (SIRT, n=13/13/1; TACE, n=15/27/3); vascular invasion (SIRT, n=14; TACE n=13); mean AFP level ug/L (SIRT, 801; TACE, 690)
- Activity calculated by BSA method
- Using RECIST and evaluated after 4 and then every 12 weeks, CR/PR/SD/PD were 0/3/11/9 for SIRT and 1/2/16/16 for TACE
- Median survival was 6.0 months for both SIRT and TACE
- No differences were found for any complications or major complications between groups. Hematologic specific complications different between treatments: SIRT had 0 and TACE had 10
B-NR
- Retrospective single-center (Italy) review of patients with locally advanced HCC/very large intermediate HCC/recurrent HCC treated with either SIRT (resin) (n=63) or sorafenib (n=74) who were SIRT eligible
- OS similar for SIRT and sorafenib
- Patient characteristic included hepatitis C/B (SIRT, n=29/9; sorafenib, n=32/11); AFP>200ng/mL (SIRT, n=22; sorafenib, n=20); prior HCC treatments (SIRT, n=32; sorafenib, n=42); no PVT (SIRT, n=32; sorafenib, n=47); Child Pugh A/B (SIRT, n=58/5; sorafenib, n=64/10); MELD (SIRT, 9; sorafenib, 9); BCLC B/C (SIRT, n=26/37; sorafenib, n=39/35)
- Sorafenib was reduced for 56 patients and interrupted for 66 patients (cancer progression, n=31; SAEs, n=27; liver failure, n=8); 33 patients received a half dose for >70% of treatment period of median 4 months.
- Activity administered was 1.71 BGq for whole liver (n=1), right/left lobe (n=26/7) or segment (n=29)
- Tumor dose was 263.2 Gy for 27 patients with complete dosimetry
- Median OS was 13.5 months, no difference was found between SIRT and sorafenib groups
- More AEs occurred in patients taking sorafenib had grade 1/2 AE (63 events) than who received SIRT (16 events), but events for grade 3/4 AE were similar (n=21 and 22)
C-LD
- Retrospective single-center case series (UK) of patients with unresectable HCC receiving SIRT with glass or resin microspheres, followed by liver resection
- All had normal bilirubin (5.0 to 17.0 mmol/L)
- Time from SIRT to resection: mean 322 days (range 195–703)
- Resected margins were R0 (n=4), R1 (n=5)
- Mean increase in FLR was 264 cm3
- Clavien-Dindo classification was II (n=5) III (n=7), IV (n=2), V (n=1)
C-LD
- Retrospective single-center (USA) analysis of 27 patients with unresectable HCC (63% HCV, 19% HBV) who underwent SIRT (resin)
- Median overall survival (OS) and liver progression-free survival (LPFS) were 11.7 months (95% CI 6.6–16.8) and 2.5 months (95% CI 1.9–3.1), respectively
- Pretreatment bilirubinemia was associated with a 2+ increase in Child-Pugh (CP) score within 3 months (P = 0.001) and 6 months (P = 0.039) of SIRT treatment
- Pretreatment bilirubinemia and transaminasemia were both associated with an increased CP class within 3 months of SIRT (p=0.009 and p=0.021, respectively)
- Pretreatment bilirubinemia and transaminasemia in HCC patients may be predictors of risk for liver function decline after SIRT treatment
C-LD
- Retrospective single-center (Belgium) analysis of 30 patients with HCC (13.3% HCV, 16.7% HBV) who were treated with SIRT (resin) after shown to be refractory to TACE with drug-eluting beads (DEB-TACE)
- Median overall survival (OS) after SIRT treatment was 14.8 months (8.33–26.5 95% CI)
- As assessed by MRI scans, a tumor response rate was achieved in 36.7% of patients at a mean of 2.9 months (range 1-6 months) following SIRT
- 10% of patients (3/30) were successfully downstaged to within Milan criteria and received liver transplants
- SIRT can be a safe and effective therapy for patients with intermediate or advanced HCC which has proven refractory to TACE
C-LD
- Retrospective single-center case series (USA) of 111 patients (59.1% HCV, 8.2% HBV) treated with SIRT (resin) for unresectable HCC
- Median overall survival (OS) was 13.1 months (95% CI, 10.3–18.4), and median survival without progression in the liver (liver PFS) was 9.8 months (95% CI, 6.8–14.8)
- A number of factors were significantly associated with longer OS. These included absence of bilobar disease, absence of PVT, early stage BCLC disease vs later stage, absence of ascites, sorafenib treatment, and treatment with other liver-directed locoregional treatments in addition to SIRT
- In 6 patients, SIRT was used as a bridge to liver transplantation, which resulted in greatly improved survival compared to patients who did not undergo liver transplants (69.0 months vs 12.1 months, respectively; p=0.001)
- 21.5% of patients experienced treatment-related adverse events (AEs) 1 week after SIRT, and 43.4% experienced these 3 months after SIRT. The most common AEs reported were abdominal pain, ascites, nausea, and edema
C-LD
- Retrospective single-center case series (Italy) of 22 patients with HCC undergoing liver transplant after SIRT with resin microspheres
- Patient characteristics included hepatitis B/C (n= 2/17); BCLC A/B/C (n=3/15/4); before SIRT within Milan criteria (n=3); at LT within Milan criteria (n=18)
- Using mRECIST, CR/PR/SD/PD was 9/9/1/2
- Median activity delivered was 1.6 GBq
- MELD score increased for 11 patients within 6 months after SIRT and remained stable for 11 patients
- AFP decreased in all cases after SIRT
- Downstaging occurred for 19 patients and 3 had successful bridge to LT
- OS from SIRT was 43.9 months and from LT was 30.2 months
13. Patients with unresectable PVTT should be treated with SIRT with palliative intent, which may lead to downstaging, followed by transplant, surgical resection, or ablative therapies.
References: SIRT with resin microspheres in Asian regions
Article
Grade
Key Points
B-NR
- Retrospective single-center (Korea) cohort study of patients with unresectable advanced HCC treated with either SIRT (resin) or SIRT with concurrent chemoradiation therapy (CCRT)
- Patient characteristics for the propensity score matching cohort included cirrhosis (SIRT, n=37; CCRT, n=35), Child Pugh B (SIRT, n=7; CCRT, n=2); BCLC B/C (SIRT, n= 12/50; CCRT, n=14/48); hepatitis B/C (SIRT, n=52/6; CCRT, n=50/2); AFP ng/mL (SIRT, n=216; CCRT, n=1291); PVT (SIRT, n=24; CCRT, n=33)
- Using mRECIST, tumor response was determined at 1, 3, 6 months and 1 year after treatment
- Response was better in the CCRT than SIRT arm at 1 month (P<0.001) but was better in the SIRT arm than the CCRT at 3 months (P=0.04)
- By 6 months no differences were detected in tumor responses
- Median OS was 14.0 for SIRT and 13.2 for CCRT (P=0.435)
- PVTT was associated with survival in multivariate analysis
- Biochemical AEs were different between treatment groups. Overall, AEs occurred more frequently in the CCRT group than in the SIRT group
B-NR
- Systematic review and meta-analysis of moderate quality RCTs and observational studies on patients with HCC with PVTT treated with SIRT (glass or resin) or sorafenib; conducted in USA, Italy, Spain, South Korea, Japan, China
- SIRT resulted in increased OS compared to sorafenib, and was more significant at 6 months and 1 year
- Kaplan–Meier rates were lower with SIRT than with sorafenib, significant at 3 months, 6 months and 1 year
- 1-year OS was significantly higher with SIRT than with sorafenib
- Pooled incidence of grade 3/4 adverse events was higher with sorafenib (28%) than with SIRT (9%) but not significant
- SIRT seemed as an effective therapeutic option for patients with HCC and PVTT
- Several factors are a significant source of heterogeneity in 1-year OS in patients undergoing SIRT: ECOG status, Child–Pugh status, extrahepatic metastasis, and previous history of HCC treatment
C-EO
- Clinical consensus statement from experts in China on HCC with PVTT
- Simultaneous diagnosis of HCC with PVTT and differentiating benign and malignant PVTT are essential. Biopsy is the gold standard but radiological examinations have also been used
- Main points to differentiate PVT from PVTT were defined
- Cheng’s classification should be used for PVTT
- Although sorafenib is the only treatment recommended by BCLC, Chinese experts suggest combinations of treatments
- Surgical resection is the first choice of treatment. Post-operative recurrence can be prevented with TACE, sorafenib, and antiviral drugs. Preoperative radiotherapy is recommended for certain patients
- SIRT is recommended for patients with non-resectable primary lesion, liver function Child-Pugh A level, and types I, II, III PVTT
- Local ablation should be used with caution in combination with other treatments
C-EO
- Clinical practice guideline by experts from Japan, Taiwan, South Korea, China, India, Pakistan, Indonesia, Philippines on HCC
- SIRT is considered for:
- Unresectable HCC: as an alternative locoregional therapy
- Patients who are not suitable candidates for TACE due to bulky tumor and/or portal vein invasion
C-EO
- Clinical consensus statement from experts in China on HCC with PVTT
- Doctors in China tend to use more curable treatments for PVTT patients
- PVTT should be diagnosed with Cheng’s classification
- Different multidisciplinary treatments are recommended taking into account liver function (Child–Pugh), resectability, extrahepatic metastasis, and extent of PVTT
- Surgery is the preferred option for patients with type I/II PVTT. Type III can undergo resection after downstaging with TACE and/or radiotherapy SIRT is recommended for patients with unresectable primary tumors; PVTT types I–III; and Child–Pugh A liver function
C-EO
- Clinical practice guideline from experts in Korea on suspicious or newly diagnosed HCC
- Staging followed mUICC system and BCLC was considered complementary
- Antiviral therapy is recommended for HBV-infected patients undergoing TACE, HAIC, resection, or EBRT
- Local ablation, TACE, and sorafenib are recommended for defined cases
- Tumor response should be assessed with mRECIST and RECIST
- SIRT can be performed safely in patients with PVTT, and outperforms TACE in downstaging HCC patients with UNOS T3 to T2
- The role of SIRT is mentioned regarding downstaging and its safety for patients with PVTT but no recommendations are made on its use
References: SIRT with resin microspheres in non-Asian regions
Article
Grade
Key Points
C-LD
- Retrospective single-center (Italy) analysis of patients with HCC BCLC-C and PVTT treated with SIRT (resin) before liver transplantation
- Etiology was hepatitis C in all 4 patients
- Median dose delivered was 1.9 GBq
- Patients with BCLC-C and PVTT were treated with SIRT to downstage prior to transplantation
- mRECIST was used to assess tumor response; 2 patients had a CR and 2 had PR
- SIRT resulted in a complete response for thrombosis within Milan criteria; only one patient was out of pathological Milan criteria
- OS was 39.1 months
C-LD
- Systematic review of RCTs, non-RCTs and observational studies of patients with HCC and PVTT
- 722 patients were treated with SIRT: 540 with glass microspheres, 160 with resin; 22 were unspecified
- Median survival was 9.7 months, median disease control rate was 74.3%
- Median OS of Child–Pugh class A patients was higher (12.1 months) than that of class B (6.1 months)
- Median OS of main PVTT patients was lower (6.1 months) than that of branch PVTT (13.4)
- Most common adverse events were fatigue, abdominal pain, and nausea/vomiting
- There is a lack of reporting Child–Pugh class and location of PVTT
- Studies lacked information on HBV and HCV status
- Adverse events were not reported in most studies
- There is insufficient evidence as to whether glass or resin microspheres are better
14. Patients with life-limiting liver-dominant disease with unresectable metastases should be treated with SIRT with palliative intent.
References: SIRT with resin microspheres in Asian regions
Article
Grade
Key Points
A
- Meta-analysis of 3 RCTs (SIRveNIB, SARAH, SORAMIC) conducted in Europe and Asia comparing SIRT (resin) with sorafenib
- SIRT is non-inferior in OS to sorafenib as first-line therapy for advanced HCC
- A total of 1243 patients with advanced HCC and the per protocol (PP) population was 933 patients
- OS was 11.0, 9.9, and 14.0 for the SIRT arms and 10.0, 9.9, 11.1 months for the sorafenib arms, respectively
- Pooled median OS for PP population was 10.2 months for SIRT and 9.2 months for sorafenib
- Superiority of SIRT to sorafenib was found for non-cirrhotic patients and patients with hepatitis B (53.7% in SIRveNIB, 5.1% in SARAH, and 10.5% in SORAMIC)
- Safety population included 1090 patients (SIRT, n=515; sorafenib, n=575)
- For SIRveNIB and SARAH, AEs and SAEs were more numerous in the sorafenib than in SIRT arm; ≥grade 3 AEs incidences was lower for SIRT than sorafenib
- For SORAMIC, addition of SIRT to sorafenib did not increase AE rate
B-R
- Multi-center open-label RTC of SIRT (resin) vs sorafenib for Asian patients with locally advanced HCC
- Liver function parameters for inclusion: total bilirubin < 2.0mg/dL; INR ≤ 2.0; ALP ≤ 5 x institutional ULN; AST and ALT ≤ 5 x institutional ULN; albumin ≥ 2.5g/dL
- No difference in OS between SIRT and sorafenib, but better safety profile for SIRT than sorafenib
- Patient characteristics included ECOG 0/1 (SIRT, n=135/47; sorafenib, n=141/37) BCLC A/B/C (SIRT, n=0/93/88; sorafenib, n=1/97/80); Child Pugh A/B (SIRT, n=165/14; sorafenib, n=160/16); hepatitis B/C/B+C (SIRT, n=93/26/4; sorafenib, n=104/19/5)
- Activity administered was calculated by BSA or partition model and mean activity was 1.8 GBq
- Response was evaluated with RECIST 1.1
- Median daily dose was 644.5 mg sorafenib for patients who were planned to receive 400 mg twice daily
- ITT Median OS was 8.8 months for SIRT and 10.0 months for sorafenib; PP median OS was 11.3 month and 10.4 months; median PFS at any site was 5.8 and 5.1 respectively
- BCLC C treated population had median OS of 9.2 months for SIRT and 5.8 months for sorafenib (P=0.0475)
- Reported AEs were 437 events for SIRT and 1031 events for sorafenib
- Fewer SIRT patients than sorafenib patients experienced one or more AEs: 78 (60.0%) of 130 patients and 137 (84.6%) of 162 patients; AEs of grade ≥ 3: 36 (27.7%) and 82 (50.6%); or serious AEs (SAEs): 27 (20.8%) and 57 (35.2%)
B-NR
- Retrospective single-center cohort study (Hong Kong) of patients with unresectable advanced HCC treated with SIRT (resin) or TACE
- Patient characteristics included BCLC A/B (SIRT, n=15/1; TACE, n=14/2); hepatitis B/C (SIRT, n=12/0; TACE, n=13/3), AFP ng/mL (SIRT, 38; TACE, 242.5); albumin g/L (SIRT, n=40; TACE n=36.5); MELD (SIRT, 7.5; TACE 8.5); no portal invasion (SIRT, n=8; TACE, n=8)
- Using mRECIST and evaluating in 2 months, CR/PR/SD/PD were 0/4/5/7 for SIRT and 0/2/5/9 for TACE
- Median OS was 19.9 months for SIRT and 14.0 months for TACE (P=0.615)
- Despite title, not all patients had HBV (75% SIRT and 81.3% TACE)
B-NR
- Retrospective multi-center (South Korea) case series of HCC patients (n=50), BCLC stages A—C (20% HCV, 66% HBV), treated with SIRT (resin)
- Portal vein invasion in 15 of 50 patients
- Study aim was to specifically evaluate safety, efficacy, and outcomes of SIRT treatment in a population of Asian patients (treated in South Korea), a majority of whom had chronic HBV infections
- 40% of patients showed a response to treatment while 46% achieved stable disease. BCLC stage was significantly associated with overall response rate (ORR) (p=0.003)
- Median overall survival (OS) for the entire cohort was 40.9 months (95% CI, 10.2–71.6 months). For patients with BCLC stage A, median survival was not reached, but the mean survival time was 39.4 months. For patients with BCLC stage B, median OS was 42.4 months (95% CI, 22.9–86 months), and for patients with BCLC stage C, median OS was 17.9 months (95% CI, 11.2–24.7 months)
- In univariate analysis, BCLC stage, Child-Pugh Score, PVT, and tumor response were significantly associated with survival
- Median time-to-progression (TTP) for the group overall was 5.9 months (range 0.9—46.1 months)
- Follow-up treatments were conducted in 31 patients due to remnant HCC or HCC progression; these follow-up treatments included TACE, RFA, surgery, radiation treatment, and combination treatments
- SIRT treatment appears to be well tolerated and effective in Asian patients with early to intermediate stage BCLC, and follow-up treatments post-SIRT were safely provided in this population
B-NR
- Meta-analysis of 2 RCTs and 9 observational studies conducted in Germany, Spain, China, Egypt, Turkey, USA: 1652 patients with unresectable HCC treated with SIRT (resin and/or glass)
- HBV: 14.1% in TACE, 12.9% in SIRT; HCV: 32.1% in TACE, 40.7% in SIRT
- Liver function was assessed and reported for each paper; no differences were found in patient characteristics among the trials
- 1-year and 2-year survival rates were analyzed based on observational or RCT study design; 1-year rates were similar, but 2-year rates were higher for SIRT than TACE treated patients
- Tumor responses were assess using either WHO (n=4) or mRECIST (n=5), the significant differences varied depending on type of analysis used (mRECIST)
- Serious AEs (≥grade 3) were rare and did not differ between treatments
B-NR
- Systematic review and meta-analysis of RCTs on intermediate and locally-advanced HCC treated with SIRT or sorafenib and conducted in France, Spain, Italy, South Korea, and Singapore
- No significant differences in OS were found between SIRT and sorafenib, although subgroup analysis of patients with PVT showed superiority of SIRT in OS
- Disease control rate was similar with SIRT and sorafenib
- SIRT resulted in significantly higher ORR (29.3%) than sorafenib (8.4%), which has been considered a bridge option before liver transplantation or surgical resection
- Sorafenib led to a higher incidence of grade ≥3 events: fatigue, weight loss, diarrhea, and hypertension
- SIRT resulted in 1.7% radiation hepatitis
B-NR
- Retrospective multi-center (Korea) cohort study of outcomes between HCC patients with PVT who were treated with SIRT (n=32, 71.9% HBV) versus sorafenib (n=31, 96.8% HBV)
- There were no significant differences in either median overall survival (OS) or time-to-progression (TTP) between the SIRT treatment group and the sorafenib treatment group (13.8 months and 10.0 months, p= 0.22; and 6.0 months and 6.0 months, p= 0.08, respectively)
No significant differences in OS (p= 0.97) or TTP (p= 0.34) were observed after inverse probability weighting (IPW) was used to adjust for differences in baseline characteristics of treatment groups - All patients in SIRT group had portal vein invasion
- Significantly more serious adverse events (grade 3 or 4) were observed in the sorafenib treatment group than in the SIRT treatment group (5/31 and 1/32; p < 0.01, respectively)
C-LD
- Retrospective single-center (Singapore) analysis of 103 patients with HCC (23.3% HCV, 47.6% HBV) treated with SIRT (resin)
- Patients were typically unsuitable for surgical resection, and typically of intermediate or advanced stage disease (BCLC B or BCLC C stage). 31.1% had portal vein invasion
- Median overall survival (OS) for the entire cohort was 14.4 months (95 % CI 11.0–22.2)
- Patients with Child-Pugh (CP) class A disease had significantly better median OS compared to patients with Child-Pugh class B disease (21.7 months vs 7.1 months, respectively; p=0.0001)
- Hepatitis C, pretreatment vascular invasion, low serum albumin, and elevated levels of total bilirubin levels were all significantly associated with poorer overall survival
- Disease control of treated lesions was 100%; however, 37% of patients eventually developed progressive disease due to the development of new lesions, local extension of tumor into the vasculature, or both
C-LD
- Prospective single-center (Singapore) case series of 24 patients with unresectable unilobar HCC treated with SIRT (resin)
- Treatment intent was palliative (n=15) or for downstaging (n=9)
- SIRT delivered via right or left hepatic artery, and liver volumes were measure prior to SIRT and 4-6 weeks and 8-6 weeks post-SIRT using CT
- Patient characteristics include portal hypertension (n=6), Child Pugh A (n=14), Child Pugh (n=10), Hepatitis B positive (n=15), BCLC-A (n=9) BCLC-B (n=9) BCLC-C (n=6), PVT (n=6)
- Total liver volume did not change over the 8 weeks; ipsilateral lobe volume decreased and FLR volume increased by 8 weeks
- A quarter of patients experienced > 20% FLR hypertrophy by 8 weeks
C-LD
- Case series analysis of 30 patients (Hong Kong) treated with SIRT (resin) for advanced inoperable HCC (6.7% HCV, 70% HBV)
- Majorities of patients had chronic HBV infection and had been on antiviral therapy >4 years
- Median overall survival (OS) was 13.2 months and median progression-free survival (PFS) was 3.3 months
- Significantly longer median OS was seen in patients without PVT compared to those with PVT (17.1 months vs 4.4 months, p=0.015); for those whose duration of alfa-feto protein (AFP) response was >6 months vs those whose AFP response was shorter (21.2 months vs 8.6 months, p=0.001); and for treatment responders vs non-responders (21.2 months vs 8.6 months; P=0.015)
- Univariate analysis identified presence of PVT, response to treatment, and duration of AFP response >6 months as prognostic factors for OS
- Univariate analysis identified prior TACE treatment, tumor volume, response to treatment, and duration of AFP response>6 months as prognostic for progression-free survival (PFS)
- Treatment-related complications developed in 56.7% of patients, with grade 3 adverse events occurring in 16.7%. No higher-grade complications were reported
C-LD
- Retrospective multi-center case series (Asia-Pacific, Europe, USA) of patients with HCC (or other malignancies) receiving SIRT with resin microspheres, followed by liver transplantation or resection
- Patient characteristics included bilobar (n=44), cirrhosis (n=41), total bilirubin grade ≥1 (n=28)
- Intent of SIRT was bridge (n=9) downstaging or palliative (n=84) or not available (n=7)
- Median IQR total SIRT activity was 1.5 GBq
- Median time to LT was 10.1 months and to surgery, 5.7 months
- Complete resection was achieved in 54 patients, R1 in 15, and R2 in 2
- 25 resected patients had exposure of the FLR to SIRT, 3 had partial exposure of the FLR to SIRT; 32 had whole liver SIRT
- 78 patients did not have post-SIRT chemotherapy
C-LD
- Retrospective single-center (Hong Kong) study of outcomes in patients with inoperable HCC who received SIRT treatment (n=30) (resin) compared to those who did not (n=16)
- HCV/HBV infection rates of patients were not specified
- MAA assessment was performed in both groups and survival time was calculated from that date
- Median overall survival (OS) was >31.9 months for patients with BCLC A stage disease, 14.5 months for patients with BCLC B, and 5.2 months for patients with BCLC C
- Among patients with BCLC C, SIRT treatment was associated with significantly longer median OS (5.2 months vs 3.8 months, p=0.047.
- SIRT was also significantly associated with longer OS among patients with PVT (5.2 months vs 3.8 months, p=0.04) and patients who had less than 3 nodules (10.6 months vs 3.3 months, p=0.004)
- Multivariate analysis identified independent factors for survival as Child-Pugh class, tumor diameter sum, BCLC stage, and SIRT treatment
- Radioembolization-induced liver disease (REILD) was reported in 13% of patients
- SIRT may improve survival for certain subgroups of patients with inoperable HCC, but caution should be taken for the possible complication of REILD
C-EO
- Clinical practice guideline by experts from Japan, Taiwan, South Korea, China, India, Pakistan, Indonesia, Philippines on HCC
- SIRT is considered for:
- Unresectable HCC: as an alternative locoregional therapy
- Patients who are not suitable candidates for TACE due to bulky tumor and/or portal vein invasion
C-EO
- Clinical consensus statement by experts from Taiwan on HCC
- BCLC should be used for prognostic prediction but other systems may be used in subgroups
- Prevention: vaccination for HBV, antiviral therapy (HBV, HCV), nucleotide/nucleoside analogues and interferon-based therapies
- SIRT is considered for:
- BCLC C stage patients with PVT
- Patients with major portal vein invasion, large tumor burden, or refractory to TACE
C-LD
- Clinical consensus statement of expert from Hong Kong on unresectable HCC
- Unresectable HCC was defined taking into account FLR
SIRT is considered for:
- Bridging to liver transplantation in suitable patients
- Multifocal or large burden tumors in Child–Pugh A patients
- Unresectable or unablatable HCC >5 cm
- Small burden HCC that failed responding to TACE in Child–Pugh A and selected Child–Pugh B patients
- Patients with vascular invasion and liver-dominant HCC in patients with Child–Pugh score ≤7 and bilirubin <2 mg/dL
- Large, bulky tumors abutting essential vascular and/or biliary structures, or when the ability to achieve adequate oncological margins is a concern
C-EO
- Clinical consensus statement from experts in Hong Kong on HCC
- SIRT with Y-90 can be considered:
- For downstaging tumors for potential subsequent resection
- For patients with post-TACE tumor progression
- As an alternative locoregional therapy for unresectable HCC
- For patients with large tumors or tumors with portal vein invasion
C-EO
- Clinical consensus statement on unresectable HCC by experts from China, Hong Kong, South Korea, Singapore, Taiwan
SIRT is considered in the following cases:
- Early-stage HCC (BCLC A): for bridging treatment for liver transplantation
- Intermediate-stage HCC (BCLC B: for bilobar, multinodular or large tumor burden, and also to treat patients after conventional TACE has failed. SIRT is also mentioned as a possible neoadjuvant treatment but there is limited data
- Advanced-stage HCC (BCLC C): for patients with vascular invasion and liver-dominant metastatic HCC
SIRT is also acknowledged as:
- Leading to favorable results regarding downsizing and objective response compared to TACE in some studies (intermediate HCC)
- Not associated with a strong embolic effect and, therefore, not contraindicated for patients with tumor thrombosis of major portal veins (advanced HCC)
Adverse events less likely with SIRT than TACE, but there are SIRT-specific complications
- SIRT contraindicated in tumor/normal liver ratios and high hepatopulmonary shunts
References: SIRT with resin microspheres in Asian regions
Article
Grade
Key Points
B-R
- Multi-center open-label RCT conducted in France on SIRT (with resin microspheres) vs sorafenib on locally advanced and unresectable HCC after unsuccessful TACE
- No significant difference in OS between SIRT and sorafenib
- Compared sorafenib 400 mg twice daily with SIRT to lobe, sector or segment
- Activity was calculated using BSA method
- Patient characteristics included hepatitis C/B (SIRT, n=55/13; sorafenib, n=49/15); ECOG 0/1 (SIRT, n=145/92; sorafenib, n=139/83); BCLC A/B/C (SIRT, n=9/66/162; sorafenib n=12/61/149); Child Pugh A(5-6)/B7/unknown (SIRT, n=196/39/2; sorafenib, n=187/35/0); bilobar (SIRT, n=50; sorafenib, n=35); macrovascular invasion (SIRT, n=149; sorafenib, n=128); AFP (SIRT, median 87 ng/mL, sorafenib, median 80.0 ng/mL)
- Activity delivered per patient was 1.394 GBq
- Median follow-up was 27.9 months in the SIRT group, 28.1 months in sorafenib group
- Response was evaluated with RECIST 1.1
- Median OS and PFS was 8.0 and 4.1 months for SIRT and 9.9 and 3.7 months for sorafenib
- Best overall response include CR (SIRT, n=5; sorafenib, n=2), PR (SIRT, n=31; sorafenib, n=21), SD (SIRT, n=93; sorafenib, n=131), PD (SIRT, n=60; sorafenib, n=44)
- 1088 serious adverse events were reported (SIRT, n=518 events; sorafenib, n=570 events)
B-R
- Multi-center open-label pilot RCT conducted in Germany on patients with unresectable HCC receiving SIRT with resin microspheres
- Patients randomized to receive either SIRT (n=13) or TACE (n=15)
- Patient characteristics included ECOG 0/1 (SIRT, n=10/3; TACE, n=12/3); Child Pugh 5/6/7 (SIRT, n=9/3/1; TACE, n=9/4/2); AFP mean (SIRT, 636 ng/dL; TACE, 2624.7 ng/dL); total bilirubin median IQR (SIRT 1; TACE 1.08); Albumin median IQR (SIRT 3.63; TACE 4.20); BCLC A/B/C (SIRT, n=5/5/3; TACE, n=4/8/3)
- Median activity 1.6 GBq delivered to whole (n=7), lobe (n=5), or segment (n=1)
- No difference in QoL measures were detected 12 weeks after treatment
- Using RECIST 1.0, PR was 30.8% for SIRT and 13.3% for TACE; 2 patients in each group were downstaged for LT (n=3) or RFA (n=1)
- Median PFS was 3.6 months for SIRT and 3.7 months for TACE
- No differences in frequency of AE between groups; only GI events occur more frequently in SIRT group; SAE occurred in 7 and 5 patients, respectively
B-NR
- Retrospective SEER analysis of 189 patients (USA) with unresectable HCC who were treated with SIRT using resin microspheres (n=77) or treated with SBRT (n=112)
- Etiology not specified
- Median overall survival (OS) for SIRT-treated patients was 12 months (95% CI: 9–17) vs 14 months (95% CI: 10–18) for patients treated with SBRT
- Disease-specific survival (DSS) for SIRT-treated patients was 14 months (95% CI: 10–22) vs 14 months (95% CI: 12–20) for patients treated with SBRT
- After adjustment for confounding factors, no significant differences were seen between treatment groups for OS (hazard ratio (HR), 0.72; 95% CI, 0.49–1.07; p=0.1077) or DSS (HR, 0.70; 95% CI, 0.46–1.05; p=0.0880)
- For both treatment groups, elevated AFP levels were significantly associated with higher risk of death (p=0.0459) and disease-specific risk of death (p=0.0233)
B-NR
- Prospective single-center (Italy) analysis of 89 patients with unresectable HCC (77.5% HCV and 7.9% HBV) who were treated with SIRT (resin). 37% of these patients had PVT
- Partial or complete response was seen in 70% of patients 3 months after SIRT treatment, and in 90.5% of patients 9 months after treatment.
- There was no significant difference in overall survival between patients with PVT and patients without PVT (p=0.672).
- At 6 months post-treatment, regression of PVT was seen in 48.1% (13/27) of patients still alive
- The presence of PVT does not appear to affect survival of patients with unresectable HCC who undergo SIRT
B-NR
- Retrospective single-center (Italy) review of patients with locally advanced HCC/very large intermediate HCC/recurrent HCC treated with either SIRT (resin) (n=63) or sorafenib (n=74) who were SIRT eligible
- OS similar for SIRT and sorafenib
- Patient characteristic included hepatitis C/B (SIRT, n=29/9; sorafenib, n=32/11); AFP>200ng/mL (SIRT, n=22; sorafenib, n=20); prior HCC treatments (SIRT, n=32; sorafenib, n=42); no PVT (SIRT, n=32; sorafenib, n=47); Child Pugh A/B (SIRT, n=58/5; sorafenib, n=64/10); MELD (SIRT, 9; sorafenib, 9); BCLC B/C (SIRT, n=26/37; sorafenib, n=39/35)
- Sorafenib was reduced for 56 patients and interrupted for 66 patients (cancer progression, n=31; SAEs, n=27; liver failure, n=8); 33 patients received a half dose for >70% of treatment period of median 4 months.
- Activity administered was 1.71 BGq for whole liver (n=1), right/left lobe (n=26/7) or segment (n=29)
- Tumor dose was 263.2 Gy for 27 patients with complete dosimetry
- Median OS was 13.5 months, no difference was found between SIRT and sorafenib groups
- More AEs occurred in patients taking sorafenib had grade 1/2 AE (63 events) than who received SIRT (16 events), but events for grade 3/4 AE were similar (n=21 and 22)
B-NR
- Retrospective single-center (Turkey) analysis of 80 patients who underwent SIRT (n=40) (resin) or TACE (n=40) for treatment of HCC (stage BCLC B or C)
- Although treatment groups were similar in most baseline characteristics, there was a significantly higher rate of chronic liver disease in the TACE treatment group (85%) than in the SIRT treatment group (55%), p=0.003. Rates of HCV/HBV infection were not given
- Mean OS Of the SIRT-treated group was significantly longer than mean OS of the TACE-treated group: 39.24±4.62 months (95% CI, 30.18–48.29 months) vs 30.63±3.68 months (95% CI, 23.42–37.84 months); p=0.014 and 2-year survival rates were 72% and 74% for the SIRT-treatment group and 47% and 59% for the TACE treatment group
- There was no significant difference between rates of disease recurrence or chronic complications between the two treatment groups
- For the SIRT treatment group, dimension of the largest lesion was a significant predictor of survival, while for the TACE treatment group, BCLC stage and female sex were significant predictors of survival
- Although there was a significantly longer mean OS for the SIRT treatment group vs the TACE treatment group, the significantly higher rate of chronic liver disease in the TACE treatment group should be considered as a factor that may influence survival
B-NR
- Retrospective multi-center (Spain) cohort analysis of patients with HCC and portal vein invasion (PVI) who were treated with either SIRT (resin) (n=26) or sorafenib (n=47) as first-line therapy
- Etiology not specified
- Median overall survival was 8.8 months (95%CI 1.8–15.8) in the SIRT treatment group and 5.4 months (95%CI 2.7–8.1) in the sorafenib treatment group (p= 0.047)
- Compared to sorafenib treatment, SIRT treatment of HCC patients with PVI resulted in a statistically significant improved survival time
C-LD
- Retrospective single-center (Lebanon) analysis of 23 Arab patients treated with SIRT (resin) for primary liver cancer or hepatic metastases from other primary cancers. Patients were treated within the setting of a private, low-volume non-referral center
- Liver malignancies represented were unresectable primary HCC (n=8, 7 of them with BCLC-C) and others
- 37.5% of HCC cases (3/8) showed chronic HCV or HBV infection
- Median overall survival (OS) from time of SIRT treatment was 12 months (range, 3-40 months)
- Median time-to-progression was 7 months (range, 3-36 months)
- Tumor responses included 5 cases of complete response, 13 partial responses, 1 stable disease, and 4 cases of progressive disease
- Median OS for the entire patient group is comparable to that of other recent studies involved mixed tumor types
- SIRT can be performed with efficacy and a low rate of complications in the “real-world” setting of a low-volume, non-referral private medical center in the Middle East
C-LD
- Retrospective single-center case series (USA) of 111 patients (59.1% HCV, 8.2% HBV) treated with SIRT (resin) for unresectable HCC
- Median overall survival (OS) was 13.1 months (95% CI, 10.3–18.4), and median survival without progression in the liver (liver PFS) was 9.8 months (95% CI, 6.8–14.8)
- A number of factors were significantly associated with longer OS. These included absence of bilobar disease, absence of PVT, early stage BCLC disease vs later stage, absence of ascites, sorafenib treatment, and treatment with other liver-directed locoregional treatments in addition to SIRT
- In 6 patients, SIRT was used as a bridge to liver transplantation, which resulted in greatly improved survival compared to patients who did not undergo liver transplants (69.0 months vs 12.1 months, respectively; p=0.001)
- 21.5% of patients experienced treatment-related adverse events (AEs) 1 week after SIRT, and 43.4% experienced these 3 months after SIRT. The most common AEs reported were abdominal pain, ascites, nausea, and edema
C-LD
- Retrospective single-center (USA) analysis of 27 patients with unresectable HCC (63% HCV, 19% HBV) who underwent SIRT (resin)
- Median overall survival (OS) and liver progression-free survival (LPFS) were 11.7 months (95% CI 6.6–16.8) and 2.5 months (95% CI 1.9–3.1), respectively
- Pretreatment bilirubinemia was associated with a 2+ increase in Child-Pugh (CP) score within 3 months (P = 0.001) and 6 months (P = 0.039) of SIRT treatment
- Pretreatment bilirubinemia and transaminasemia were both associated with an increased CP class within 3 months of SIRT (p=0.009 and p=0.021, respectively)
- Pretreatment bilirubinemia and transaminasemia in HCC patients may be predictors of risk for liver function decline after SIRT treatment
C-LD
- Retrospective single-center (Belgium) analysis of 30 patients with HCC (13.3% HCV, 16.7% HBV) who were treated with SIRT (resin) after shown to be refractory to TACE with drug-eluting beads (DEB-TACE)
- Median overall survival (OS) after SIRT treatment was 14.8 months (8.33–26.5 95% CI)
- As assessed by MRI scans, a tumor response rate was achieved in 36.7% of patients at a mean of 2.9 months (range 1-6 months) following SIRT
- 10% of patients (3/30) were successfully downstaged to within Milan criteria and received liver transplants
- SIRT can be a safe and effective therapy for patients with intermediate or advanced HCC which has proven refractory to TACE
C-LD
- Retrospective single-center case series (Italy) of 22 patients with HCC undergoing liver transplant after SIRT with resin microspheres
- Patient characteristics included hepatitis B/C (n= 2/17); BCLC A/B/C (n=3/15/4); before SIRT within Milan criteria (n=3); at LT within Milan criteria (n=18)
- Using mRECIST, CR/PR/SD/PD was 9/9/1/2
- Median activity delivered was 1.6 GBq
- MELD score increased for 11 patients within 6 months after SIRT and remained stable for 11 patients
- AFP decreased in all cases after SIRT
- Downstaging occurred for 19 patients and 3 had successful bridge to LT
- OS from SIRT was 43.9 months and from LT was 30.2 months
C-LD
- Retrospective single-center (Spain) case series of 25 patients with unresectable HCC and PVT were treated with SIRT (resin)
- Etiology not specified
- No significant liver-related side effects were seen at 1- and 2-months post-treatment
- Overall median survival time was 10 months (95% CI, 6.6-13.3 months)
- Controlled disease was seen in 66.7% of patients at 2 months and 50% of patients at 6 months
- SIRT treatment may offer a favorable risk/benefit profile for patients with unresectable HCC and PVT
C-LD
- Single-center (Italy) case series analysis of survival and prognostic factors for 43 patients with unresectable HCC (46.5% HCV, 11.63% HBV, 2.32% HCV+HBV) treated with SIRT (resin)
- Median overall survival (OS) from start of treatment was 27.7 months (SE = 3.044, 95% CI 15.75–27.68 months) and median progression-free survival (PFS) was 16.8 months (SE = 2.873, 95% CI 11.13–22.39 months)
- Factors significantly associated with longer median OS were absence of PVT (p = 0.0241; R = 2.0835), higher pre-treatment hemoglobin (HBG) values (p = 0.0471; R = -0.3397), and tumor lesions numbering less than 3 (p = 0.0155; R = 1.6520)
- Common hepatic artery use as a release site was associated with the most frequent presentation of remote adverse events (p = 0.039)
- Activity administered dose was associated with intra-procedural toxicity (p = 0.039)